Testicular cancer is the leading cancer among individuals assigned male at birth from ages 15 to 35. A key symptom in testicular cancer is a painless lump in the testicle. Since testicular cancer is rare, but can be fatal, an early diagnosis and treatment can significantly enhance the cure rate.
What is Testicular Cancer?
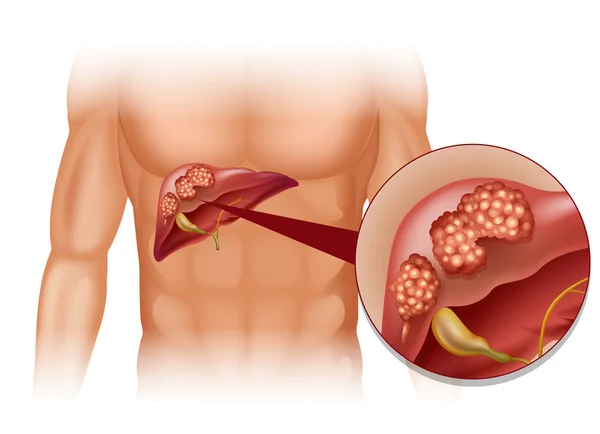
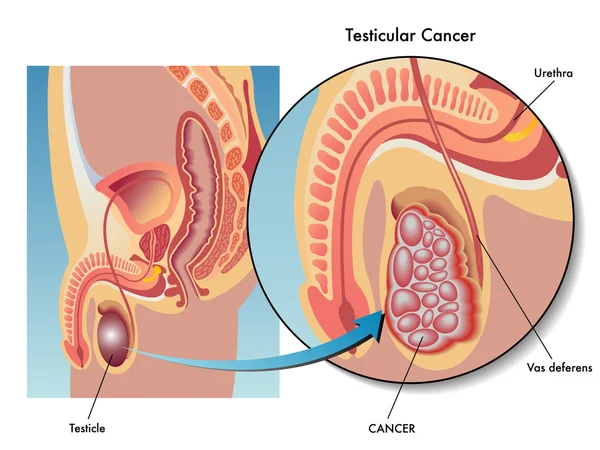
Testicular cancer occurs when cancerous cells grow in the tissues of one or both testicles. Testicles are two walnut-sized glands housed in the scrotum, a skin pouch located beneath the penis, that are responsible for producing sperm and the hormone testosterone. Like all cancers, testicular cancer is a serious illness, but it is often highly treatable and can be cured.
Types of Testicular Cancer
Approximately 90% of testicular cancers originate from germ cells. There are two main types:
– Seminoma: A slow-growing cancer typically affecting individuals in their 40s or 50s.
– Non-seminoma: Faster-growing and more common in late teens to early 30s. This category includes embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma.
Some tumors can be a combination of seminoma and non-seminoma.
Prevalence
Though rare (affecting about 1 in every 250 males) testicular cancer is the most prevalent cancer in the 15-35 age group for those assigned male at birth.
Symptoms and Causes of Testicular Cancer
Signs and Symptoms
A painless lump in the testicle is the most common indication of testicular cancer. Other symptoms include:
– Swelling or fluid buildup in the scrotum
– Feeling of heaviness in the scrotum
– Dull ache in the groin or lower abdomen
– Pain in the scrotum or testicle
– Shrinking of a testicle
These symptoms may also appear in other conditions; so a thorough medical evaluation is crucial to avoid delayed diagnosis and treatment.
Causes and Risk Factors
Cancer develops as cells multiply abnormally, but exact causes remain unclear. Germ cells are typically involved.
Key risk factors include:
– Age: Primarily affects males from ages 15 to 35.
– Undescended Testicles: A lack of descent into the scrotum may increase risk.
– Race/Ethnicity: Higher incidence in non-Hispanic white males.
– Family History: A genetic predisposition may exist.
– Infertility: Potentially linked (though not fully understood.)
Diagnosis and Tests
Diagnostic Approach
Your healthcare provider may diagnose testicular cancer after investigating a lump or other changes in your testicle that you discovered during a self-exam. Sometimes, it is identified during a routine physical examination.
Common procedures and tests used to diagnose testicular cancer include:
– Physical Exam and History: Your provider will ask about your symptoms and conduct a thorough examination to look for signs of testicular cancer. This includes feeling for lumps in your testicles and checking your lymph nodes for signs of cancer spread.
– Ultrasound: If your provider detects any abnormalities during the exam, they will likely order an ultrasound. This painless procedure uses high-energy sound waves to create images of the tissues inside your body.
– Inguinal Orchiectomy and Biopsy: If the ultrasound suggests the presence of cancer, your provider may remove the affected testicle through an incision in your groin. A specialist will then examine the tissue under a microscope to look for cancer cells.
Other tests that may be conducted include:
– Serum Tumor Marker Test: This blood test measures levels of specific substances associated with certain types of cancer, known as tumor markers. For testicular cancer, common markers include alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG or beta-HCG), and lactate dehydrogenase (LDH). Different tumors may elevate different markers; for example, seminomas may raise HCG (but not AFP), while non-seminomas may raise AFP (but not HCG). Elevated LDH levels may suggest cancer spread.
– CT Scans, X-Rays, and MRIs: A CT scan uses X-rays to create detailed images of the inside of your body. Your provider may order a CT scan of your abdomen and pelvis to check for cancer spread to abdominal organs, or a standard X-ray to look for spread to your lungs. If there is suspicion of spread to your central nervous system (brain and spinal cord), an MRI may be performed. An MRI utilizes magnets and radio waves to create images of the body’s interior.
What are the stages of testicular cancer?
Understanding the stages of testicular cancer is important for treatment planning. Stages include:
– Stage 0: Abnormal cells confined to testicles.
– Stage I: Cancer within the testicle.
– Stage II: Spread to abdominal lymph nodes.
– Stage III: Further spread to lymph nodes or organs.
Management and Treatment
Treatment Options
Treatment considers health, preferences, stage, and type of tumor. Seminomas favor radiation, while chemotherapy suits both types.
– Surgery: Removal of the cancerous testicle is standard.
- Radical Inguinal Orchiectomy: Testicle removal via groin incision.
- Retroperitoneal Lymph Node Dissection (RPLND): May follow orchiectomy in non-seminomas for cancer staging or treatment.
– Radiation Therapy: Targets seminomas post-surgery.
– Chemotherapy: Uses drugs to kill cancer cells, effective for both seminoma and non-seminoma tumors.
Prevention
While testicular cancer isn’t preventable, conducting monthly self-exams is recommended to detect changes early.
Outlook and Prognosis
Regular self-exams and early treatment significantly improve outcomes. Although testicular cancer is not typically preventable, self-awareness and timely medical advice are key to successful management.
Living With Testicular Cancer
Regular follow-ups and lifestyle adjustments post-treatment aid in long-term recovery and monitoring. Discuss any concerns or symptoms with healthcare providers to maintain health and well-being.